Communication: Are the Right People Telling the Right Information to the Right Patients?
| What do patients want to know? | Fertility is of great importance to many people diagnosed with cancer
Patients may have questions, but are not sure who/when to ask.
|
| How are we doing? Does the current model work? | In general, patients are not satisfied with fertility preservation communication:
Pre-consultation knowledge is low:
Post-consultation knowledge is also poor:
Decisional Conflict:
|
| When should FP be discussed, and who is responsible for doing this? | ASCO guidelines about fertility preservation10
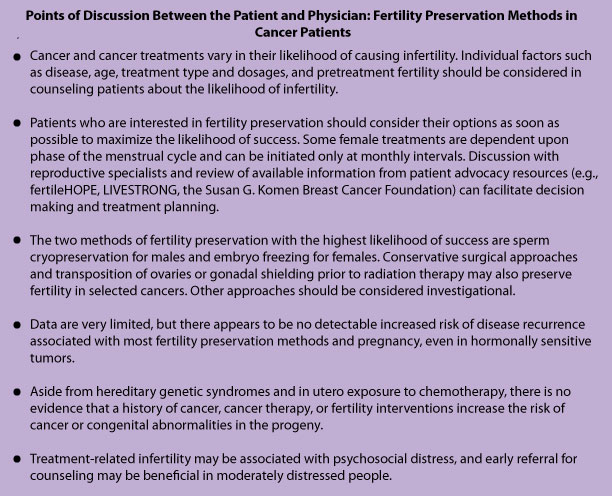
The American Society of Clinical Oncology had a multi-disciplinary panel issue guidelines in 2005 stating:
Early referral to a reproductive specialist is essential Patients who were referred prior to (rather than after) surgery, were more likely to have an earlier start to the COS cycle, earlier start to chemotherapy, and the option for a 2nd COS cycle (if desired)12. Points of Discussion between the Oncology Team and the Patient:
Table adapted from Lee SJ, Schover LR, Partridge AH, et al: American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol 24:2917-31, 2006. |
| Can we improve educational methods about FP? |
|
References
- Schover LR, Rybicki LA, Martin BA, et al: Having children after cancer. A pilot survey of survivors’ attitudes and experiences. Cancer 86:697-709, 1999
- Saito K, Suzuki K, Iwasaki A, et al: Sperm cryopreservation before cancer chemotherapy helps in the emotional battle against cancer. Cancer 104:521-4, 2005
- Partridge AH, Gelber S, Peppercorn J, et al: Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol 22:4174-83, 2004
- Meneses K, McNees P, Azuero A, et al: Development of the Fertility and Cancer Project: an Internet approach to help young cancer survivors. Oncol Nurs Forum 37:191-7
- Thewes B, Meiser B, Rickard J, et al: The fertility- and menopause-related information needs of younger women with a diagnosis of breast cancer: a qualitative study. Psychooncology 12:500-11, 2003
- Balthazar U, Fritz MA, Mersereau JE: Fertility preservation: a pilot study to assess previsit patient knowledge quantitatively. Fertil Steril 95:1913-6, 2011
- Peate M, Meiser B, Friedlander M, et al: It’s Now or Never: Fertility-Related Knowledge, Decision-Making Preferences, and Treatment Intentions in Young Women With Breast Cancer–An Australian Fertility Decision Aid Collaborative Group Study. J Clin Oncol 29:1670-7
- Balthazar U, Fritz MA, Mersereau JE: Fertility preservation treatment options: What do patients actually understand about their choices? Fertility and sterility 94:S104, 2010
- Balthazar U, Fritz MA, Mersereau JE: Decision making under duress: What predicts decisional conflict among fertility preservation patients? Fertility and sterility 94:S105, 2010
- Lee SJ, Schover LR, Partridge AH, et al: American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol 24:2917-31, 2006
- Quinn GP, Vadaparampil ST, Lee JH, et al: Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol 27:5952-7, 2009
- Lee S, Ozkavukcu S, Heytens E, et al: Value of early referral to fertility preservation in young women with breast cancer. J Clin Oncol 28:4683-6
- King L, Quinn GP, Vadaparampil ST, et al: Oncology nurses’ perceptions of barriers to discussion of fertility preservation with patients with cancer. Clin J Oncol Nurs 12:467-76, 2008
- Thewes B, Meiser B, Taylor A, et al: Fertility- and menopause-related information needs of younger women with a diagnosis of early breast cancer. J Clin Oncol 23:5155-65, 2005
About the Author
Jennifer Mersereau, MD, MSCI, is an reproductive endocrinologist in the University of North Carolina’s Department of Obstetrics and Gynecology. As the Director of the Fertility Preservation Program, she has extensive experience guiding patients and physicians through the oncofertility experience.
This page was last updated: March 14, 2012.