Educating Providers on Evidence-Based Medical Guidelines is a chapter of Oncofertility Communication: Sharing Information and Building Relationships across Disciplines where the authors, Lauren N.C. Johnson and Dr. Clarisa R. Gracia, outline previous medical paradigms and how they have changed to incorporate new evidence-based medical guidelines in fertility preservation and oncofertility.
 The old paradigm of medical practice relied heavily on individual clinical experiences and the knowledge of pathophysiology. Based on this, physicians would refer to text books and senior colleagues when faced with a difficult patient situation. As such, many patient care decisions were influenced by provider bias rather than objective data. In the late twentieth century, there was a paradigm-shift to focus on evidence-based medicine which highlighted the critical importance of objective data in medical decisions. Evidence-based medicine (EBM), as a whole, is a tool for solving clinical questions. The original definition of EBM was “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients” and was later amended to include the critical role of the patient in health care decisions. Now, EBM is “the integration of the best available research evidence with clinical expertise and patient values” which allows for the best clinical decisions relating to patient care.
The old paradigm of medical practice relied heavily on individual clinical experiences and the knowledge of pathophysiology. Based on this, physicians would refer to text books and senior colleagues when faced with a difficult patient situation. As such, many patient care decisions were influenced by provider bias rather than objective data. In the late twentieth century, there was a paradigm-shift to focus on evidence-based medicine which highlighted the critical importance of objective data in medical decisions. Evidence-based medicine (EBM), as a whole, is a tool for solving clinical questions. The original definition of EBM was “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients” and was later amended to include the critical role of the patient in health care decisions. Now, EBM is “the integration of the best available research evidence with clinical expertise and patient values” which allows for the best clinical decisions relating to patient care.
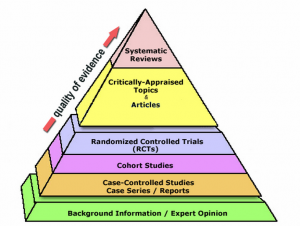
In an effort to generate appropriate information, clinicians focus on the “PICO” model: P stands for Patient, Problem, or Population; I stands for Intervention; C stands for Comparison; O stands for Outcome. These four areas allow for clinicians to focus their questions in a logical way that allows for quicker literature searches and data gathering. Beyond the PICO model, grading systems were put in place to help medical professionals evaluate the quality of the evidence in a particular study or set of guidelines through grades of “good, fair, or poor”. Even further beyond these systems, many clinicians refer to the Strength-of-Recommendation Taxonomy (SORT) system which focuses mainly on patient-centered outcomes, quality of life, and symptom improvement. Recently, researchers have expressed increased interest in the impact of cancer therapies on fertility as more cancer patients become long-term survivors. As Oncofertility has garnered more attention and interest, the quality of data relating to fertility preservation has drastically improved from simple case studies to randomized controlled trials. Based on the quality of the data available, the American Society of Reproductive Medicine (ASRM) reclassified oocyte cryopreservation to be an established technique. This is a prime example of how EBM can transform clinical care.
The Oncofertility Consortium relies heavily on EBM and is dedicated to providing clinicians with access to educational resources through various avenues. The Consortium hosts an annual conference with didactic sessions as well as hands-on, small-group training courses, frequent ‘Virtual Grand Rounds‘ and online access to currently published research studies. Practice guidelines for fertility preservation in cancer patients have been published by several professional societies including the American Society for Clinical Oncology (ASCO), ASRM, and the British Fertility Society. Some organizations, such as ASCO, ASRM, and The Endocrine Society, even offer Continuing Medical Education credits (CME) for online training modules.
As Oncofertility continues to rapidly evolve, knowledge of Evidence Based Medicine, and access to high-quality, patient-oriented literature, will allow physicians to consistently offer excellent care to patients seeking fertility preservation. The Oncofertility Consortium will continue to share resources with our large network and promote the role of EBM in fertility preservation through our Annual Conference, Virtual Grand Rounds, among many other channels.


 By: Brigid Martz Smith -
By: Brigid Martz Smith -