 Education materials, whether in print or web-based, have a large role in helping patients feel confident in their medical decision-making. Continuing with our overview of Oncofertility Communication: Sharing Information and Building Relationships across Disciplines, Chapter 3 focuses on the importance of education, and the role of decision-making tools, within the Oncofertility community. The authors, Dr. Gwendolyn P. Quinn, Dr. Susan T. Vadaparampil, Ivana Sehovic, MPH, and Dr. Marla L. Clayman outline that the majority of adolescent young adult patients choose not to take steps to preserve fertility but overwhelmingly appreciate the discussion about potential fertility issues. But how does a cancer patient make the decision of whether or not to pursue fertility preservation? Chapter 3, Patient and Family Tools to Aid in Education and Decision-Making About Oncofertility, dives into the three components of decision-making, (1) risk appraisal (2) information integration and (3) long-term considerations.
Education materials, whether in print or web-based, have a large role in helping patients feel confident in their medical decision-making. Continuing with our overview of Oncofertility Communication: Sharing Information and Building Relationships across Disciplines, Chapter 3 focuses on the importance of education, and the role of decision-making tools, within the Oncofertility community. The authors, Dr. Gwendolyn P. Quinn, Dr. Susan T. Vadaparampil, Ivana Sehovic, MPH, and Dr. Marla L. Clayman outline that the majority of adolescent young adult patients choose not to take steps to preserve fertility but overwhelmingly appreciate the discussion about potential fertility issues. But how does a cancer patient make the decision of whether or not to pursue fertility preservation? Chapter 3, Patient and Family Tools to Aid in Education and Decision-Making About Oncofertility, dives into the three components of decision-making, (1) risk appraisal (2) information integration and (3) long-term considerations.
Risk appraisal includes not only physical risks such as the effect of treatment delay on cancer outcomes and the risks associated with the fertility preservation procedures themselves, but also the psychological risks. How will the patient feel if she is unable to have biological children and did not take steps to preserve her fertility? Risk appraisal often goes hand-in-hand with the second component of decision making; information integration. This involves the patient processing information about fertility preservation options, medical procedures, associated costs, as well as religious, ethical or moral concerns about these options. The third component, long-term considerations, relates to retrieving the stored sperm, embryos, oocytes or tissue. How will the patient feel about using artificial reproductive technology to achieve a pregnancy? How will their partner feel about having a child with donor sperm or eggs?
Patients facing such complex fertility preservation decisions can benefit from the use of decision aids. The International Patient Decision Aids Standards (IPDAS) criteria for what constitutes a patient decision aid are quite specific . The aids must 1) provide facts about the patient’s condition, options and features, 2) help people clarify their values (the features that matter most to them), and 3) help people share their value with their healthcare practitioner and others.
Chapter 3 provides examples of quality decision-making tools, ranging from Oncofertility 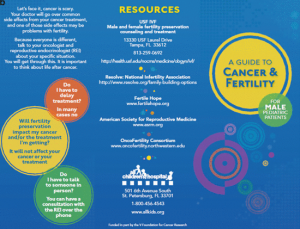 booklets to websites such MyOncofertility.org. These represent decision-making tools that were developed with multidisciplinary teams and with a scientific approach. While these are, in no way, a replacement for a discussion with a medical professional, decision-making tools can offer patients and their families peace of mind about their choices.
booklets to websites such MyOncofertility.org. These represent decision-making tools that were developed with multidisciplinary teams and with a scientific approach. While these are, in no way, a replacement for a discussion with a medical professional, decision-making tools can offer patients and their families peace of mind about their choices.
Take the time to review Chapter 3 of Oncofertility Communication and share with your colleagues. If you have decision-making tools in your clinic or office, consider reviewing them based on the criteria outlined by IPDAS and see if they need to be edited or clarified for patients. And please continue to explore the Oncofertility Consortium website for available brochures and information for clinicians and patients alike.


 By: Brigid Martz Smith -
By: Brigid Martz Smith -