Ovarian Tissue Cryopreservation (OTC)
| Who are appropriate candidates? |
Ovarian tissue cryopreservation is usually only considered in certain cases:
- Patients who do not have time to undergo controlled ovarian stimulation (COS) for embryo or oocyte cryopreservation. COS is the more mature technology and should be the first-line treatment if time allows.
- Patients who are planning surgery for another reason may be good candidates for ovarian tissue cryopreservation. Specifically, this may include women planning an oophrectomy as part of their treatment for endometrial cancer, etc.
- Pre-pubertal girls who do not have the option of COS.
- OTC is generally not recommended in women who:
- are >41 years old
- have a large ovarian cyst on the ovary to be cryopreserved
- have received prior chemotherapy that has significantly impaired ovarian function

|
| What is the National Physician’s Cooperative (NPC)? |
What is the NPC?
- Many centers around the country are members of the NPC, centered at Northwestern University.
- The goals of the NPC, with respect to OTC, involve providing research tissue for a national research repository that can be used to:
- Optimize techniques for freezing and thawing of ovarian tissue for use in transplant or in vitro follicle maturation (IFM).
- Investigate factors affecting successful maturation of immature follicles obtained from ovarian tissue including the use of 3-dimensional biogel scaffolds, growth factors, hormones and other culture conditions.
- Determine the efficacy of ovarian cryopreservation techniques.
- Provide long term follow up on patients who have ovarian tissue frozen for their own use.
- A substantial portion of the patient’s tissue will be cryopreserved and reserved for her own use.
How can you become involved?
- Step-by-step instructions on how to become a member of the NPC are located on the NPC page.
- Once your site is a member of the NPC, the initiation of an OTC program involves several steps, as detailed on the NPC Members page.
|
| Pregnancies from OTC? |
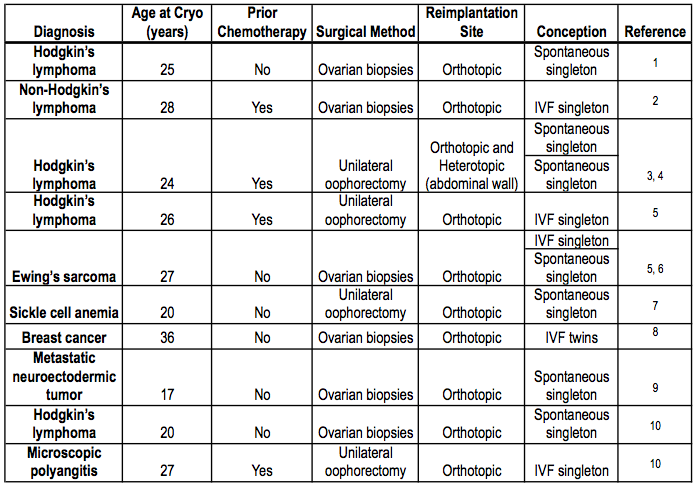
It is important to emphasize that OTC is experimental, and that a very limited number of pregnancies have resulted from this technology. The following table gives a summary of live births after autologous transplantation of cryopreserved-thawed ovarian tissue.
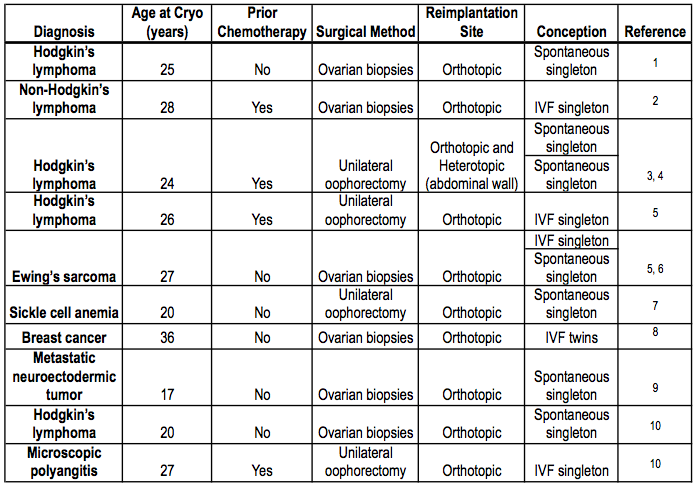
Table adapted from Laxmi A. Kondapalli, Ovarian Tissue Cryopreservation and Transplantation. Cancer Treat Res. 2012 (In press).
Transplantation
- While there have been some pregnancies and live-births after allografting ovarian tissue between identical and non-identical sisters10, transplantation is generally not regarded as a safe option for women with cancer.
- One study, looking at autopsy files, ovarian metastasis was found in 8-4-55.5% of women younger than 40 years old11. Certain types of cancers had higher rates of metastasis than others (gastric cancer – 55%, leukemia – 8.4%).
- Given that there are no reliable methods to detect minimal residual disease in the cryopreserved tissue, the safety of transplantation is in question.
In vitro maturation
- For cancer patients, the general recommendation is to avoid transplantation of ovarian tissue in cases where there is concern about reseeding cancer cells, and instead, to consider in vitro maturation of oocytes.
- Researchers at the Oncofertility Consortium are working on in vitro maturation of oocytes, using follicle culture with alginate hydrogels.
- They are working with cell cultures, animal models, and translation research with human tissue, with the hope of developing a protocol to allow quiescent oocytes to grow in vitro to the point of fertilization.
- See our Oncofertility Methods page for the most up-to-date progress of the Oncofertility Consortium.
- To date, in humans, there has not been successful fertilizations or pregnancies from this technique.
|
| Special Circumstances with OTC |
Turner Syndrome
- One study found that ovarian tissue biopsied from girls with Turner Syndrome had identifiable follicles in 26% of the cases12.
- Factors that were associated with increased likelihood of finding follicles included mosaic karyotype, normal FSH levels, AMH levels above 2 pmol/liter, spontaneous menses, and spontaneous puberty.
- It is unknown if follicles identified in these patients will be able to produce viable oocytes.
Donating 100% of ovarian tissue for research
- Some women who are planning to have one or both ovaries removed may opt to donate 100% of their ovarian tissue to research, if they are not interested in future fertility.
- Usually, a modification of an IRB application and consent from is needed for these instances.
|
References
1. Donnez J, Dolmans M, Demylle D, et al. Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet 2004;364:1405-10.
2. Meirow D, Levron J, Eldar-Geva T, et al. Pregnancy after transplantation of cryopreserved ovarian tissue in a patient with ovarian failure after chemotherapy. New England Journal of Medicine 2005;353:58-63.
3. Demeestere I, Simon P, Emiliani S, Delbaere A, Englert Y. Fertility preservation: successful transplantation of cryopreserved ovarian tissue in a young patient previously treated for Hodgkin’s disease. Oncologist 2007;12:1437–42.
4. Demeestere I, Simon P, Moffa F, Delbaere A, Y E. Birth of a second healthy girl more than 3 years after cryopreserved ovarian graft. Human Reproduction 2010;25:1590-1.
5. Andersen CY, Rosendahl M, Byskov AG, Loft A, Ottosen C, et al. Two successful pregnancies following autotransplantation of frozen/thawed ovarian tissue. Human Reproduction 2008;23:2266-72.
6. Ernst E, Bergholdt S, Jorgensen JS, et al. The first woman to give birth to two children following transplantation of frozen/thawed ovarian tissue. Human Reproduction 2010;25:1280-81.
7. Roux C, Amiot C, Agnani G, Aubard Y, Rohrlich PS, et al. Live birth after ovarian tissue autograft in a patient with sickle cell disease treated by allogeneic bone marrow transplantation. Fertil Steril 2008;93:e15-2413.e19.
8. Sánchez-Serrano M, Crespo J, Mirabet V, et al. Twins born after transplantation of ovarian cortical tissue and oocyte vitrification. Human Reproduction 2010;93:e11–3.
9. Donnez J, Squifflet J, Jadoul P, et al. Pregnancy and live birth after autotransplantation of frozen-thawed ovarian tissue in a patient with metastatic disease undergoing chemotherapy and hematopoietic stem cell transplantation. Fertility and Sterility 2011;95:e1-4.
10. Donnez J, Silber S, Anderson CY, Demeestere I, Piver P, Meirow D et al. Children born after autotransplantation of cryopreserved ovarian tissue. A review of 13 live births. Ann Med. 2011;43(6):437-50.
11. Kyono K, Doshida M, Toya M, Sato Y, Akahira J, Sasano H. Potential indications for ovarian autotransplantation based on the analysis of 5,571 autopsy findings of females under the age of 40 in Japan. Fertil Steril; 93:2429-30.
12. Borgstrom B, Hreinsson J, Rasmussen C, Sheikhi M, Fried G, Keros V et al. Fertility preservation in girls with turner syndrome: prognostic signs of the presence of ovarian follicles. J Clin Endocrinol Metab 2009;94:74-80.
About the Author
Jennifer Mersereau, MD, MSCI, is an reproductive endocrinologist in the University of North Carolina’s Department of Obstetrics and Gynecology. As the Director of the Fertility Preservation Program, she has extensive experience guiding patients and physicians through the oncofertility experience.
This page was last updated March 14, 2012.