Logistics and Safety of Pregnancy After Cancer
Reports about pregnancy after cancer treatments are rather limited. This may be because the proportion of reproductive aged women with cancer is relatively low. In addition, cancer survivors may not attempt pregnancy, due to fertility problems (amenorrhea) and/or fear of recurrence.
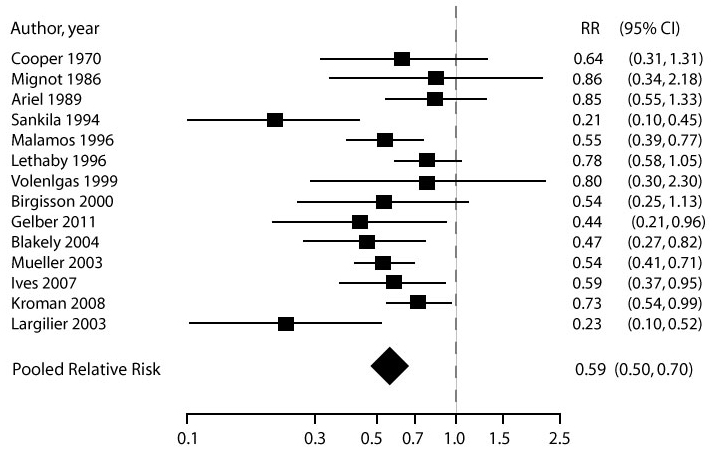
| Safety of pregnancy: recurrence risk | The available data, generally reported in retrospective cohort studies, does NOT indicate an increased risk of recurrence of cancer in women who become pregnant after cancer. This holds true even in women with hormone sensitive cancers, like breast cancer.
Overall survival analysis of women who became pregnant after cancer. Adapted from Azim HA, Jr., Santoro L, Pavlidis N, et al. Safety of pregnancy following breast cancer diagnosis: a meta-analysis of 14 studies. Eur J Cancer;47:74-83. |
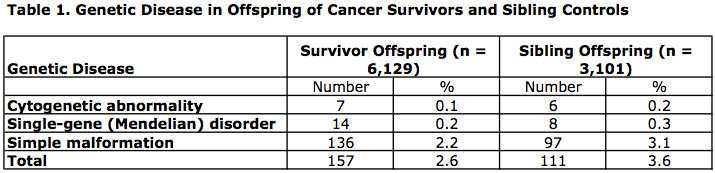
| Safety of pregnancy: offspring | One of the largest studies evaluating pregnancy outcomes in cancer survivors compared reproductive outcomes in men and women who had a history of childhood cancers as compared to their siblings3.
Adapted from Green DM, Sklar CA, Boice JD, Jr., et al. Ovarian failure and reproductive outcomes after childhood cancer treatment: results from the Childhood Cancer Survivor Study. J Clin Oncol 2009;27:2374-81.
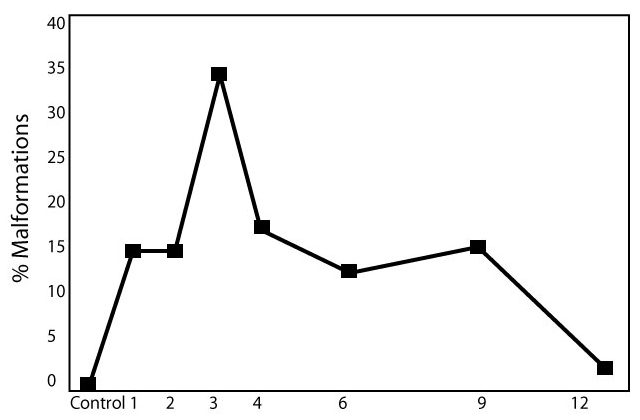
Incidence of malformations in the fetuses of mice mated at different time intervals (1-12 weeks) following injection with cyclophosphamide (75 mg.kg). Adapted from Meirow D, Epstein M, Lewis H, Nugent D, Gosden RG. Administration of cyclophosphamide at different stages of follicular maturation in mice: effects on reproductive performance and fetal malformations. Hum Reprod 2001;16:632-7. |
| Timing of pregnancy | Data is limited about when it is safe to consider pregnancy after treatment for cancer. This decision is usually made in close collaboration between the patient, the oncology team, and the fertility specialist.
|
References
- Ives A, Saunders C, Bulsara M, Semmens J. Pregnancy after breast cancer: population based study. BMJ 2007;334:194.
- Azim HA, Jr., Santoro L, Pavlidis N, et al. Safety of pregnancy following breast cancer diagnosis: a meta-analysis of 14 studies. Eur J Cancer;47:74-83.
- Green DM, Sklar CA, Boice JD, Jr., et al. Ovarian failure and reproductive outcomes after childhood cancer treatment: results from the Childhood Cancer Survivor Study. J Clin Oncol 2009;27:2374-81.
- Meirow D, Epstein M, Lewis H, Nugent D, Gosden RG. Administration of cyclophosphamide at different stages of follicular maturation in mice: effects on reproductive performance and fetal malformations. Hum Reprod 2001;16:632-7.
About the Author
Jennifer Mersereau, MD, MSCI, is an reproductive endocrinologist in the University of North Carolina’s Department of Obstetrics and Gynecology. As the Director of the Fertility Preservation Program, she has extensive experience guiding patients and physicians through the oncofertility experience.
This page was last updated March 14, 2012.