Alpha-Mannosidosis
| Prevalence | The prevalence of alpha-mannosidosis is not precisely known. It is estimated that alpha-mannosidosis occurs in approximately 1 in 500,000[1] to 1 in 1,000,000 live births and is expected to be found in every ethnic group[2]. |
| Natural History | 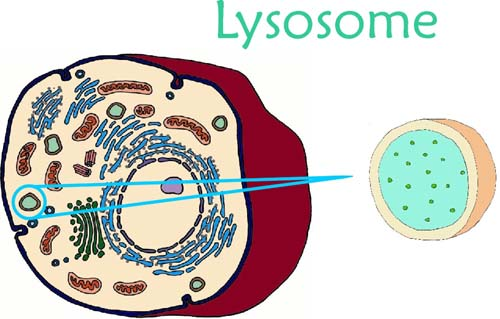 Alpha-mannosidosis is a rare-lysosomal storage disorder than is inherited in an autosomal recessive manner due to mutations in MAN2B1. MAN2B1 encodes alpha-mannosidase, a lysosomal enzyme responsible for the degradation of N-linked oligosaccharides, or more specificially, alpha-mannosidase breaks down a sugar molecule called mannose. Individuals with alpha-mannosidosis have a deficiency of alpha-mannosidase leading to immune deficiency, facial and skeletal abnormalities, hearing impairment, and mental retardation[3]. Alpha-mannosidosis is a rare-lysosomal storage disorder than is inherited in an autosomal recessive manner due to mutations in MAN2B1. MAN2B1 encodes alpha-mannosidase, a lysosomal enzyme responsible for the degradation of N-linked oligosaccharides, or more specificially, alpha-mannosidase breaks down a sugar molecule called mannose. Individuals with alpha-mannosidosis have a deficiency of alpha-mannosidase leading to immune deficiency, facial and skeletal abnormalities, hearing impairment, and mental retardation[3]. |
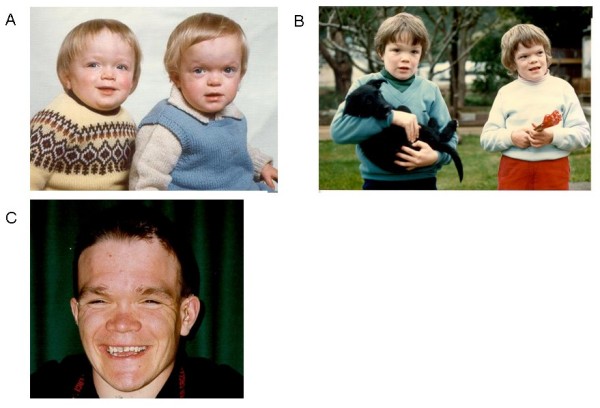
| Disease Presentation | Alpha-mannosidosis is a progressive disorder that can vary in severity. Individuals with the most severe form of the condition experience hepatomegaly and early childhood death due to recurrent severe infections. In contrast, those with the attenuated form have slow disease progression into adulthood with hearing loss and mental retardation.
The EU consortium HUE-MAN (working towards the development of an effective enzyme replacement therapy for human alpha-mannosidosis) conducted a longitudinal study on alpha-mannosidosis and thoroughly assessed the disease presentation[3]. Characteristics of the disease include:
|
| Effect on Fertility | Heamatopoietic stem cell transplant (HSCT) is the standard therapeutic option, and currently the only clinically available treatment option, for alpha-mannosidosis[6]. Given the rarity of alpha-mannosidosis, HSCT use is based on limited safety and efficacy data in humans. The largest experience with HSCT for lysosomal storage diseases exists in Hurler syndrome, for which good long-term neurodevelopmental outcomes have been demonstrated.
Grewal et al. (2004) presented four patients, aged 3-23 years, who underwent HSCT and experienced intellectual function stabilization, hearing improvement to normal or near normal for speech frequencies (3/4 patients), no development of new skeletal abnormalities, and normalization of leukocyte enzyme activity. HSCT, therefore, is capable of halting the progressive cognitive loss in patients with alpha-mannosidosis when early diagnosis occurs[8]. Mynarek et al. (2012) conducted a retrospective multi institutional analysis of 17 patients diagnosed with alpha-mannosidosis at a median age of 2.5 (1.1-23) years who underwent HSCT at a median age of 3.6 (1.3-23.1) years. At a median follow-up of 5.5 years, 88%, or 15 patients, were alive. The other two did within 5 months of HSCT. After HSCT, patients made developmental progress and most improved hearing. One patient, now an adult, has been reported to live an independent life. The retrospective study found that HSCT may be a feasible therapeutic option to promote mental development in individuals with alpha-mannosidosis[9]. Anytime HSCT use is considered, the benefits must be weighed against the overall risk of procedure related morbidity and mortality. Additionally, benefits are greater in younger patients, prior to development of disease complications. Therefore, HSCT is an option for children with alpha-mannosidosis during the first decade of life[10]. A well established risk of HSCT conditioned with total body irradiation (TBI) and high doses of gonadotoxic drugs is infertility[11].
HSCT conditioning often involves TBI and/or gonadotoxic drugs, both of which are associated with a high risk of ovarian failure in females[11,12]. The majority of female patients who are treated with TBI experience gonadal failure. In fact, 10% experience recovery of gonadal function and only 1.3% acheive pregnancy[11]. Vatanen et al. (2013) evaluated long-term ovarian function after allogenic HSCT in childhood and adolescence in 70 prepubertal female tranplant survivors and 22 adult transplant survivors (transplant occuring between 1987-2000; mean age of 9 years; age range 1-19 years). Results showed that 40/70 prepubertal females experienced spontaneous puberty, based onbreast development, and 30/70 experience spontaneous menarche. They found that there was a high risk of ovarian failure with conditioning TBI or Bu-based regimes prior to HSCT and intensive anti-leukemia therapy prior to HSCT, including CRT, decreased the possibility of spontaneous menarche.
TBI and gonadotoxic drugs are typically used to condition patients prior to HSCT, both of which lead to absence of spermatozoa. In fact, TBI is the main cause of azoospermia in patients treated with HSCT. This is due to the fact that spermatogenic stem cells are more sensitive to chemotherapy and radiation than later stage germ cells, preventing the generation of newsperm cells[11]. Rovo et al. (2013) conducted a European Group for Blood and Marrow Transplantation (EBMT) large retrospective analysis of men who underwent HSCT and found that 81% of males receiving TBI presented withazoospermia and only 1% had normal sperm counts in follow-up spermanalysis. Anserini et al. (2002) found that azoospermia is less frequent in patients conditioned with busulphan and cyclophosphamide (50%) and uncommon in those treated with cyclophosphamide alone. Suggesting, perhaps, that busulphan and cyclophosphamiade or cyclophosphamide alone may affect fertility less than traditional HSCT conditioning with TBI and gonadotoxic drugs. |
| Fertility Preservation Options | Female Fertility Preservation The risk of premature ovarian failure (POF) and infertility is very high after HSCT, however fertility issues may not become relevant for transplant survivors until a later timepoint. Therefore, fertility preservation discussions should be discussed with all young women of childbearing age and parents of children facing HSCT[15]. The risk of premature ovarian failure (POF) and infertility is very high after HSCT, however fertility issues may not become relevant for transplant survivors until a later timepoint. Therefore, fertility preservation discussions should be discussed with all young women of childbearing age and parents of children facing HSCT[15].
The main fertility preservation options available for women include: embryo cryopreservation, oocyte cryopreservation, and ovarian tissue cryopreservation. However, given that children with alpha-mannosidosis are prepubertal, they cannot undergo the necessary ovarian stimulation needed for embryo and oocyte cryopreservation. Therefore, ovarian tissue cryopreservation and autotransplantation should be considered prior to HSCT in children with alpha-mannosidosis. Ovarian Tissue Cryopreservation Alternatively, females with alpha-mannosidosis may wish to use donor ooctyes or consider adoption.
Given the risk of azoospermia is very high after HSCT, fertility preservation options should be discussed with all young men of reproductive age and parents of children facing HSCT[11]. Children with alpha-mannosidosis are typically prepubertal at the time of HSCT and prepubertal males cannot produce semen for cryopreservation. Testicular tissue cryopreservation is currently the only option for prepubertal males at high risk for infertility interested in preserving future fertility[16]. Ginsberg et al. (2014) consented 57 families to testicular biopsy, and 28 children underwent the procedure with 1 experiencing a post-operative side effect. Parents who faced this fertility preservation option at their child’s diagnosis reported they made an informed decision and carefully weighed the risks and benefits of testicular tissue cryopreservation. Testicular Tissue Cryopreservation Alternatively, males with alpha-mannosidosis may choose to use donor sperm or consider adoption. |
| Patient Fact Sheet | Print the Oncofertility Consortium® Fertility Preservation Patient Fact Sheet on Alpha-Mannosidosis to provide to your patients and their families who are considering fertility preservation prior to HSCT treatment. This fact sheet is tailored specifically to the fertility needs of children with Alpha-Mannosidosis.
Alpha-Mannosidosis Fertility Preservation Patient Fact Sheet |
References
[1] Meikle, P., Ranieri, E., Simonsen, H., Rozaklis, T., Ramsay, S., Whitfield, P., . . . Hopwood, J. (2004). Newborn screening for lysosomal storage disorders: clinical evaluation of a two-tier strategy. Pediatrics, 114, 909-916.
[2] Meikle, P., Hopwood, J., Clague, A., & Carey, W. (1999). Prevalence of lysosomal storage disorders. JAMA, 281, 249-254.
[3] Beck, M., Olsen, K., Wraith, J., Zeman, J., Michalski, J., Saftig, P., . . . Malm, D. (2013). Natural history of alpha mannosidosis a longitudinal study. Orphanet J Rare Dis, 8, 88.
[4] Malm, D., Pantel, J., & Linaker, O. (2005). Psychiatric symptoms in alpha-mannosidosis. J Intellect Disabil Res, 49, 865-871.
[5] Halperin, J., Landis, D., Weinstein, L., Lott, I., & Kolodny, E. (1984). Communicating hydrocephalus and lysosomal inclusions in mannosidosis. Arch Neurol, 41, 777-779
[6] Prasad, V., & Kurtzberg, J. (2010). Cord blood and bone marrow transplantation in inherited metabolic diseases: scientific basis, current status and future directions. . Br J Haematol, 148, 356-372.
[7] Wall, D., Grange, D., Goulding, P., Daines, M., Luisiri, A., & Kotagal, S. (1998). Bone marrow transplantation for the treatment of alpha-mannosidosis. J Pediatr, 133, 282-285.
[8] Grewal, S., Shapiro, E., Krivit, W., Charnas, L., Lockman, L., Delaney, K., . . . Peters, C. (2004). Effective treatment of alpha-mannosidosis by allogeneic hematopoietic stem cell transplantation. J Pediatr, 144, 569-573.
[9] Mynarek, M., Tolar, J., Albert, M., Escolar, M., Boelens, J., Cowan, M., . . . Sykora, K. (2012). Allogenic hematopoietic SCT for alpha-mannosidosis: an analysis of 17 patients. Bone Marrow Transplant, 47(3), 352-359.
[10] Malm, D., & Nissen, O. (2008). Alpha-mannosidosis. Orphanet J Rare Dis, 3, 21.
[11] Tichelli, A., & Rovo, A. (2013). Fertility issues following hematopoietic stem cell transplantation. Expert Rev Hematol., 6(4), 375-388.
[12] Vatanen, A., Wilhelmsson, M., Borgstrom, B., Gustafsson, B., Taskinen, M., Saarinen-Pihkala, U., . . . Jahnukainen, K. (2013). Ovarian function after allogenic hematopoietic stem cell transplantation in childhood and adolescence. Eur J Endocrinol, 170(2), 211-218.
[13] Rovo, A., Aljurf, M., Chiodi, S., S, S., Salooja, N., & G, S. (2013). Ongoing graft-versus-host disease is a risk factor for azoospermia after allogeneic hematopoietic stem cell transplantation. A survey of the late effect working party of the European Group for Blood and Marrow Transplantation.Haematologica, 98(3), 339-345.
[14] Anserini, P., Chiodi, S., Spinelli, S., Costa, M., Conte, N., Copello, F., & Bacigalupo, A. (2002). Semen analysis following allogenic bone marrow transplantation. Additional data for evidence-based counselling. Bone Marrow Transplant, 30(7), 447-451.
[15] Jadoul, P., & Donnez, J. (2012). How does bone marrow transplantation affect ovarian function and fertility? Curr. Opin. Obstet. Gynecol., 24(3), 164-171.
[16] Ginsberg, J., Li, Y., Carlson, C., Gracia, C., Hobbie, W., Miller, V., . . . Kolon, T. (2014). Testicular tissue cryopreservation in prepubertal male children: An analysis of parental decision-making. Pediatr Blood Cancer.
About the Author
Allison Goetsch, MS, CGC is a pediatric genetic counselor at Ann and Robert H. Lurie Children’s Hospital of Chicago and a member of the Oncofertility Consortium administrative core team. She completed her graduate thesis with Dr. Teresa K. Woodruff researching oncofertility and hereditary breast and ovarian cancer (HBOC) syndrome. Allison’s primary goals are to increase fertility preservation awareness and education for both health care providers and patients regarding malignant and non-malignant diseases (and/or treatments) which threaten fertility.
This page was last updated February 6th, 2016.



 Female Fertility
Female Fertility Male Fertility
Male Fertility Male Fertility Preservation
Male Fertility Preservation